Fuelling the Ambitions of Middle East (GCC) Healthcare by Getting the Basics Right
Dr Hasham Khan & Dr Urooj Khan
The Middle East is a diverse region comprising countries with varying economic development, healthcare systems, and healthcare infrastructure. In the last few decades, all the GCC states have made substantial investments in their respective healthcare sectors, leading to advancements in medical technology, improvement in healthcare facilities, capability development and building pockets of excellent clinical practice in the region. However, the region struggles with ageing infrastructure, inadequate resources, insufficient funding, workforce challenges and disparities in healthcare accessibility.
The COVID pandemic highlighted the need for different capacity building initiatives for the stakeholders, especially the need to upgrade the existing infrastructure and enhancing workforce.
Key Challenges:
The GCC healthcare sector is undergoing a transformation journey which is aspirational in its vision, scale and pace resulting in significant growth in the last 5 years. With an increasing population and a rising number of elderly people with varying and evolving healthcare needs, the region faces unique challenges in providing high quality healthcare services that are holistic in nature, offer good accessibility and affordable for all sections of the society.
The GCC states have been at the forefront of adopting new technologies and transforming the health systems to address the concerns of rising costs of care, addressing the needs of ageing population, staff, tackling workforce dissatisfaction, driving value-based-healthcare and most importantly patient centricity and satisfaction.
Example Improvement Programmes:
It promises to be a very exciting journey from a centralised, ministry owned/led, hospital centric health system to a patient centred system which began with the modernisation and digitalisation of healthcare in the last decade.
Introducing population health management and utilising population and patient data will drive improvements in decision-making, activating patients through a patient centred approach with the commitment of shifting from centralised care provision to more personalised medicine and eventually precision medicine.
This, however, is only one aspect of the transformation journey. The corporatisation of healthcare entities, along with private sector participation will result in the transformation of public sector finances, introducing costing, coding and revenue cycle management. A cultural shift from fee for service to capitated budgets and the establishment of Accountable Care Organisations or health clusters with the overall responsibility of addressing the health and care needs of their populations is another vital transformation.
Overview of Saudi Vision 2030:
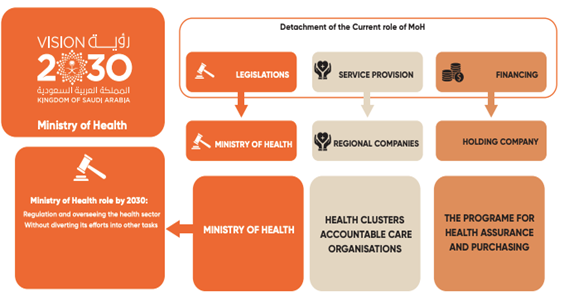
The transformation journey has also introduced several new entities and players with clearly defined roles for the provision of health care. A national payer has also been introduced along with the national regulator for universal health insurance.
Then there are entities such as Value in Care and Academic Health Councils which are attempting to answer the most vital question of value-based care and improving the effectiveness of targeted intervention through a causative link between academic research and front-line delivery along with strong clinical governance and accountability across the care continuum. The once omnipotent Health Ministries appear increasingly likely to take on their principal roles of the oversight monitors and regulators.
In a historic milestone marking the inaugural Health Day at the 28th UN Climate Change Conference (COP28), global leaders united in endorsing the health and climate change declaration, sounding the alarm on the severe health implications of climate change. The declaration underscores the urgent need to confront the connections between climate change and health.
The Road from Population Health Management to Patient Activation and Patient centred care – the era of Sharing Medicine
Population health management is the process of improving clinical health outcomes of a defined group of individuals through improved care coordination and patient engagement supported by appropriate financial and care models. This approach has been at the centre of all the transformation programmes in the GCC health economies in the last decade.
All these programmes began with the development and introduction of new models of care, a comprehensive multi-prong approach designed to improve accessibility, patient activation and a marked improvement in care outcomes.
Population health management brings health concerns into focus and addresses ways that resources can be allocated to improve the health of a group of people. It is an interdisciplinary, customisable approach that allows health departments to connect practice to policy for change to happen locally. In other words, there are partnerships within community sectors such as public health, industry, academia and local government working together to achieve positive health results.
Patient centred care means working together with an individual to plan their care and support to meet their unique needs. This cuts down the risk of negative, unfair, or harmful treatment and neglect. The individual is put at the centre, able to choose and control how they want their care and support to be.
Personalised and precision medicine falls at the other end of the spectrum. It is an emerging practice of medicine that uses an individual’s genetic profile to guide decisions made regarding the prevention, diagnoses, and treatment of disease. This knowledge of the individual’s genotype (genetic profile) can help health care planners and front-line clinicians in providing advanced diagnosis, treatment options and personalised and preventive programmes tailored to an individual’s unique genetic makeup. It will also help to predict and prevent present and future genetic diseases better and implement new therapies for rare and chronic diseases.
Example of Patient Centred Care:

The health authorities in GCC states use the genomic data to develop healthcare strategies that address the population’s specific needs now and, in the future, and support the advancement of preventive medicine in the countries.
Personalised medicine is being advanced through the data from Human Genome Projects such as the Emirate Genome Programme. This national project aims to use genomic data to improve the health of the Emirati population. The project involves scientific study and research aimed at profiling and determining the gene sequencing among UAE Nationals to aid in the prevention and treatment of chronic diseases.
It is a voluntary programme which invites Emirati citizens to take part in the study by visiting one of the sample collection sites and providing a single blood sample. The programme uses advanced sequencing technology and artificial intelligence to generate and analyse a comprehensive genome data and produce a reference genome specific to UAE citizens.
The term ‘patient activation’ implies a range of measures used to increase the active participation of patients in decision-making care. There is a large body of research and evidence that shows that patients are becoming increasingly active in the understanding of their conditions, which is readily available through various channels. It is therefore imperative that clinicians enter this doctor-patient relationship with an open mind and must start treating their patients as equal partners. The most important step to take is to assume that patients are confident provided they are given the right information expressed in the right way and to ensure they get that information where and when they need it.
Linea’s Approach to Transformation:

The new era in the doctor-patient relationship has arrived, facilitated or perhaps driven by the mobile phone, but health services and professionals are often behind the pace. They need to move to a new culture in which all data is presented in an evidence-based way, for example using the Fact Box methodology. The new era has been called the era of Sharing Medicine, which demands an empathic care and may capture the spirit better than the term personalised medicine, which still implies that the clinician is in charge. In fact, healthcare involves an emphasis on what people do for themselves.
The primary care system is the backbone of healthcare in the new age of care delivery. Most GCC health systems have inadequate primary care systems. The GCC is dependent on expatriate doctors for medical services. Limited resources and infrastructure have impacted the overall system because of a lack of access, delayed diagnosis, and mismanagement. Thus, in most countries, satisfaction with primary care services has been low.
With poor access to primary care facilities and a lack of gatekeeping, hospital utilisation continues to be very high. At least a third of emergency room service utilisation could have been avoided with better and earlier diagnosis at the primary care level. More than 2/3 of inpatient admissions are for management and treatment of chronic conditions rather than for surgical procedures, this often leads to long in-hospital stays, adversely impacting overall utilisation of resources and poor health outcomes.
Even today, a significant proportion of the healthcare expenditure in the region is spent in secondary and tertiary care hospitals, thereby aggravating, and leaving unaddressed issues related to primary care, extended care, home care, and other clinical services. The health systems must commit to increased investment in primary care both in terms of infrastructure development for fit for purpose health centres and workforce development leading to a responsible, highly skilled, trained and adaptable workforce that is able to empathise with the patients and understand their ongoing and future needs.
This is the vision for the future, which is unfolding before us now, amid all this rapid change it is vital to analyse and determine the future role of clinicians in such a modern health system.
There is a definite shift emerging in the doctor patient relationship, a shift in power from clinician to patient, a need to individualise evidence from randomised controlled trials and genetic analysis, while appreciating the need to remember, and sometimes rediscover, empathy.
All forms of individualised medicine (patient-centred, personalised, precision medicine, etc.) share one thing; They all require that practitioners understand the patients’ symptoms, needs, and aims. Essentially, empathy is a necessity. Not only is empathy required for any form of care that focuses on applying population evidence to individuals, but it can independently enhance important patient outcomes.
Most attention has been focused on the changing role of the patient, but the more dramatic change may be needed in the role of the clinician and the driver may be technological as well as social with the disruptive technology being the Internet or, its ubiquitous manifestation, the smartphone.
Patients now have access to almost all the knowledge that doctors can access, and furthermore, patients often have more time than clinicians due to ever increasing demands on the clinician’s time. But this is only part of the shift that technology is bringing about. The implications of Artificial Intelligence and cognitive computing are profound and resources like ChatGPT and other LLMs are emerging as disruptive technologies with big implications for specialties such as Pathology and Radiology as well as for specialties that are based on the face-to-face consultations such are general and family medicine that have changed little since even before the original telephone, never mind the smartphone.
The GCC healthcare industry has been grappling with many challenges, some of which include the high dependency on imports for pharmaceutical products, surgical equipment and implants, medical devices and most vitally a highly trained and skilled clinical workforce and healthcare leaders.
Another very significant challenge is the burgeoning cost of care delivery, the region like others is not immune from the impact of climate change on healthcare and the catastrophic costs of dealing with new and upcoming global pandemics will seriously test the readiness of the health systems in GCC.
The transformation journeys, emergence of disruptive technologies and new ways of working offer a glimpse of what the future may look like for both patients and doctors in the GCC as infectious diseases and lifestyle related health disorders continue to challenge the region. The constant push to adopt new & advance technologies in clinical practice and care delivery can also exert pressure on the clinicians who are constantly stressed, over worked, and burnt out.
So how can the policy makers and healthcare leaders in GCC go about addressing all the above challenges while driving the ambitions of delivering truly world class modern healthcare systems? The answer to that may not always be a radical shift towards modernisation, be the development of firm foundation upon which to build healthcare organisations of the future.
Business Improvement specialists, such as Linea, play a pivotal role in supporting the dynamic and rapidly evolving healthcare sector in the GCC.
As the healthcare landscape undergoes transformative changes, we utilise our extensive expertise and specialised knowledge to assist GCC healthcare entities in optimising operational efficiency, implementing innovative technologies, and navigating complex regulatory frameworks. In addition, we provide strategic guidance on adapting to new healthcare models, improving patient outcomes, and enhancing overall organisational resilience.
Additionally, our teams provide insights into data analytics, helping healthcare providers harness the power of information to make informed decisions, optimise resource allocation, and improve patient care. In leveraging our expertise, the healthcare sector in GCC states can navigate the challenges of change more effectively and ensure sustainable growth in an era of transformation.
To find out more about the support we can offer your organisation, contact a member of the team who will be happy to help.
t: +44 (0) 124 442 1095
Article also published in Healthcare World Magazine, issue 12, January 2024
Click below to chat to a team member